Break the Stigma Seattle: The Importance of Talking About Mental Health During Mental Health Awareness Month

Encourage those struggling or in crisis to call 988 for help.
By Dr. Carl Janzen, Associate Director of Primary Care, for Optum located in Seattle.

Seattle, known for its coffee culture, great restaurants and vibrant tech scene, is also home to a growing concern: mental health. As Seattleites confront life’s challenges, like all Americans, they face unique obstacles that impact their well-being.
Many are struggling with mental health issues such as increased anxiety and depression. According to The Centers for Disease Control and Prevention (CDC), during late June of 2020, 40 percent of U.S. adults reported they were struggling with mental health issues or substance use. These abnormally high numbers have disproportionately affected younger adults, racial and ethnic minority groups, essential workers, and unpaid adult caregivers.
Locally, like adults, youth are struggling too. Although a Washington State Healthy Youth Survey in 2023 shows that the number of youths in King County struggling with mental health issues is on a slight decline, there is still room for improvement. According to the survey, the number of 10th graders feeling like they have no one to turn to when depressed in King County is still 9.6% compared to 12.3% statewide.
Furthermore, those with depressive feelings is 23.5% locally compared to 29.9% statewide, and those feeling nervous, anxious and on edge are 60% compared to 61.7% statewide. Data Dashboard – Healthy Youth Survey (askhys.net)
Poor mental health among adolescents can impact many areas of a teen’s life and increase stress on families. Making sure teens feel connected to school and family is very important in helping them grow into healthy adulthood.
May is recognized as Mental Health Month, an opportunity to learn about mental health conditions and treatment options. Although exploring mental health treatment options, which includes psychotherapy (also known as talk therapy), medication, or self-care, can be confusing or difficult, is an important part of mental health care. Some important messages to remember this Mental Health Month are:
- You are not alone. Millions of people in the U.S are affected by mental illness each year. By acknowledging how common mental illness is, we can better understand its impact and reduce the stigma.
- Self-care such as practicing yoga or meditation, eating well-balanced meals, staying physically active and getting plenty of sleep, are healthy ways to help cope with stress so you can better take care of yourself and in turn, be in a better position to help take care of others.
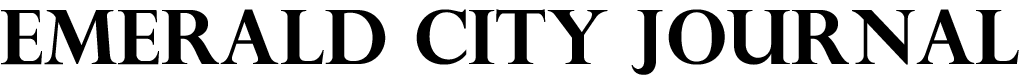
- Connect with others by talking to people that you trust about your concerns and how you are feeling. Conversation is a powerful coping tool that may help manage stress and help promote resilience.
- Consider talk therapy, which may be an appropriate option for you. Telemedicine can be a tremendous help to people particularly for people who are unable to get in-person treatment.
- Educate yourself by talking to your doctor or using online resources. The more you know, the more you can dispel misinformation or myths that can increase the stigma around mental illness and hold people back from receiving the treatment they need.
- Talk to your child about mental health. Feeling connected to family and school can have a significant impact on their mental health, so communicating openly and honestly with your child provides them with a sense of connectedness.
- If someone you know needs help, listening to them in a comfortable and non-judgmental way can be a good place to start. It’s important to genuinely express your concern and avoid blaming, criticizing, minimizing or assuming things about their experience.
- If you or someone you know is struggling or in crisis, help is available. Call or text 988, or chat 988lifeline.org to reach the 988 Suicide & Crisis Lifeline.
- Optum Disclaimer: If you or someone you know have thoughts about suicide, seek help right away. If you or someone you know is in immediate danger, call 911 or go to the closest emergency room.
Mental Health Month is a good time to have discussions about mental health and do your part to break the stigma.